CBD oil (cannabidiol) products have become very popular since being legalized in 2018. Things like CBD oil or CBD balm are well-known with people who have chronic pain due to chronic inflammation, but why? Is CBD good for inflammation? Not only yes, but absolutely yes. Did you know using CBD for inflammation issues is one of the most effective treatments that involve CBD use. The anti-inflammatory effects of CBD are backed by studies, and thousands upon thousands of user testimonials.
Despite it growing in popularity, a lot of people are still not sure what hemp derived CBD products are, if they are legal, and what real benefits they have. CBD oil products are used as a solution for a lot of different issues, only one of them being chronic inflammation relief.
TL;DR – There is scientific evidence via studies, trials, and reviews which shows that CBD can help ease bodily issues that revolve around inflammation.
How Does CBD Help With Inflammation in the Body?
Our bodies contain what is called an endocannabinoid system. Cannabidiol, or CBD, interacts with this system. This system serves many different functions that we won’t cover in this article, because it would take far too long.
The few things I will mention about it, is that it is made up of a number of different cannabinoid receptors. They are known as cannabinoid receptors CB1 and CB2.
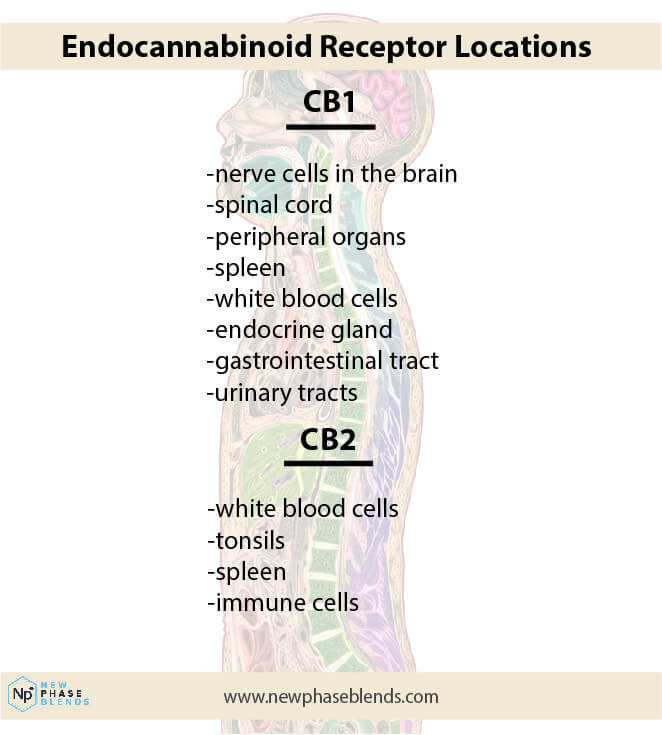
These receptors are located all over the body, including immune cells within the immune system, and even the central nervous system. Immune cells that are part of the immune system find a way to an area in our bodies that has been damaged and actually cause inflammation to protect and heal the area.
Most people don’t realize that inflammation plays a key role in the healing process. Sometimes, it’s necessary.
Related: Taking CBD for Muscle Pain
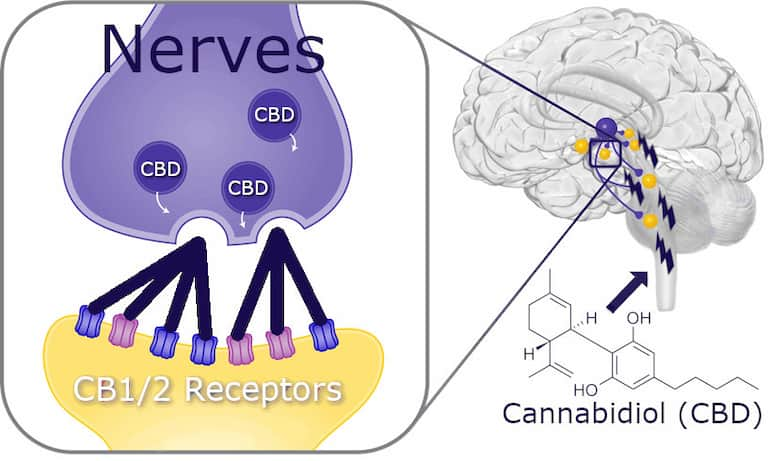
Cannabinoids, like CBD, can regulate (both directly, and indirectly) these receptors to aid in a number of different responses. For example, CBD binds indirectly to receptors, while THC binds directly.
One of these responses are in the form of anti inflammatory effects that can alleviate chronic inflammation in certain parts of our bodies. This is why using CBD for joint pain relief is so popular these days.
For example, transdermal cannabidiol reduces inflammation exceptionally well. There are also many other types of CBD products we will get into later on.
There is a lot we still need to find out about our endocannabinoid system, but we’re on the right track when it comes to clinical trials and further CBD research.
Exploring Cannabidiol (CBD)
Before having a look at different CBD products, it’s important to understand what it is. Cannabidiol, or CBD, is one of the most active compounds found in the cannabis plant.
Related: Does CBD Work?
Remember, the cannabis plant species contains both the marijuana and hemp plant. Many people don’t realize this.
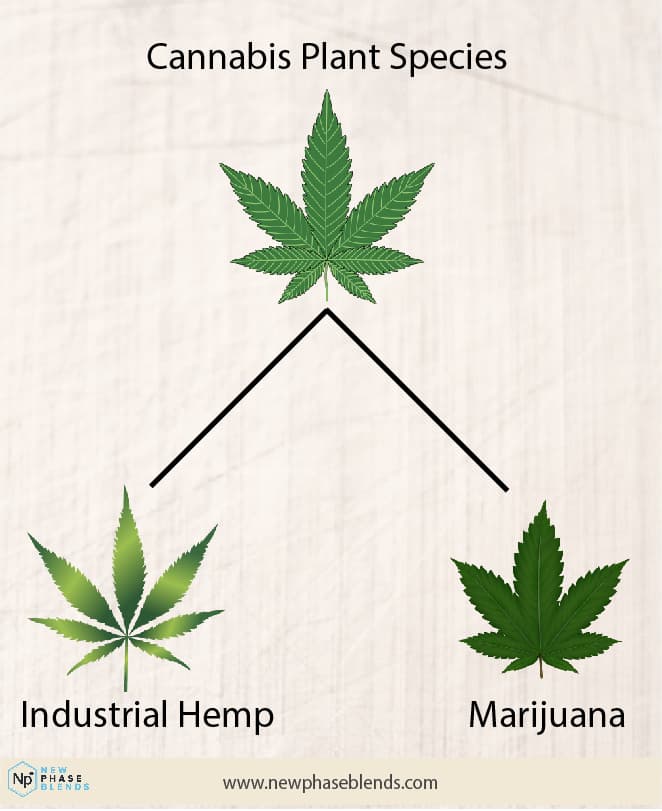
Another active compound that’s well-known because of the psychoactive properties is tetrahydrocannabinol, or THC. Clinical data shows us this is the compound in marijuana that makes people high.
Since CBD is a hemp plant derived anti inflammatory, you do not have to worry about getting high. Legally, hemp plants cannot contain more than 0.3% THC content, which is no where near enough to even get you remotely high. It will not happen.
Despite being non-psychoactive, CBD products still have many of the same medical benefits that THC has. You’re able to take advantage of all the benefits it comes with without having to deal with the feeling of being high afterwards, like with THC.
Related article: Differences Between THC and CBD
CBD exhibits many of the same benefits that medical cannabis does, just remember, it comes without the high that medical cannabis comes with. If you’re living in a state that hasn’t legalized medical marijuana, then you’ll still be able to benefit from industrial hemp derived CBD.
In order to be sure, it’s advisable to check on what your state’s laws are regarding CBD products.
Is CBD Good For Inflammation?
Despite how much CBD is growing in popularity, research on its effectiveness is still at the early stages. There’s a lot that’s still yet to be known but the current results are good. Most studies want to find a natural way to help symptoms like rheumatoid arthritis pain. Arthritis pain, unfortunately, is one of the most common inflammatory issues older adults have.
According to research, CBD is highly effective in reducing inflammation through acting on the activity in the body’s endocannabinoid receptors.
It’s effective for both acute and chronic inflammation. A study conducted on rats showed that CBD reduces chronic inflammation in rats that are suffering from osteoarthritis.
Using CBD for Inflammation That Causes Pain
If you’ve never used CBD for pain and inflammation treatments before, you should start with a considerably low dosage then gradually increase your dose.
Discover: Hemp Oil for Pain
Different CBD items vary when it comes to the actual content each contains. Be very cautious when you’re switching dose forms or starting a new package.
It’s important you take it slow regarding the dose you consume so that you know how your body reacts to the effects of CBD, and can avoid or minimize any possible, yet rare, negative reactions.
There have been a wide range of pure CBD oil dosages that have been tested in different clinical trials. However, more evidence is required in order for safe and effective dose recommendations to be made for different uses, like treating chronic inflammation. You just need to follow the recommended dose on each product unless you are given the go-ahead by a doctor to take larger doses.
What Else Might CBD Help With?
People use CBD for more than simply inflammation relief. Clinical data shows us that CBD contains a wide range of biological functions, including anti inflammatory properties that may aid with chronic inflammation.
Sure, while CBD reduces inflammation well, there are other potentials in CBD for the treatment of diabetes, heart disease (including stroke, high blood pressure, atherosclerosis and high cholesterol), inflammatory bowel disease, rheumatoid arthritis, and anxiety.
There hasn’t been a lot of research done regarding CBD, but the results of research that has already been conducted are quite promising.
According to some research, it has the ability to help with different mental health conditions in disorders related to anxiety, schizophrenia, addiction, and PTSD (post-traumatic stress disorder).
Apart from the mental benefits, it has also been found to be effective in dealing with physical conditions. CBD anti-inflammatory products may be used to treat pain that arises from arthritis and the topical balms and creams reduce inflammation.
Related: The Best Arthritis Cream
Other conditions that CBD has been proven to help with include seizures and childhood epilepsy. It also has anticancer properties and helps with managing the side effects associated with cancer treatment.
Enjoying your reading so far? Sign up to become part of the NPB community and receive a free eBook, 20% off your next order, and access to ton of educational information about cannabinoids like CBD and Delta 8. NPB hosts, arguably, the largest collection of cannabinoid info on the internet. There is no better place to learn than our educational databse.
Different Forms of CBD for Inflammation
There are different forms of CBD available for anti inflammatory effects. You can easily choose the method that fits your needs. Some of the common forms include:
Creams and Lotions
CBD infused topicals are usually meant to help with relieving both muscle and joint pain. Some can also be used for treatment of skin conditions such as psoriasis and eczema. Unlike CBD tinctures, the creams and lotions are meant to be applied directly to the skin.
Discover: CBD Cream for Back Pain
Capsules and Pills
CBD capsules are mainly used to treat digestive problems and seizure disorders. Ensure you only consume products that are approved by the Food and Drug Administration (FDA). All CBD oils, capsules, pills, really anything you buy from New Phase Blends is guaranteed to be completely legal.
Oils and Tinctures
CBD tinctures are usually liquids primarily infused with CBD oils. They’re taken by placing them under the tongue using a dropper. They’re ingested orally because the oral mucosa has many capillaries that quickly absorb the compounds. If you aren’t able to take pills and capsules, oils and tinctures are a good alternative. CBD oil can also help manage chronic inflammation, just in a slightly different manner.
Discover: 1,000 mg CBD Tinctures
Edibles
Edible CBD products are very easy to consume since they’re tasty. One of the most popular forms of edibles are gummies. They have a number of advantages including: they’re discrete, tasty, affordable and easy to travel with.
Is CBD Legal?
In the United States, hemp-derived CBD products are 100% federally legal. The caveat is that CBD oil brands need to make sure their products contain less than 0.3% THC to remain legal. Approved nonprescription CBD products should be labeled “contains less than 0.3% THC” and come with a QR code that links to a third party lab report. This lab report will show the cannabinoid content (CBD is an example of one cannabinoid) of that particular batch.
However, CBD that’s derived from marijuana and has high amounts of THC, is only legal in the states that have currently legalized recreational marijuana. This is because THC is still included as part of the controlled substances act.
Most states require participation in their medical marijuana program, which requires things like a medical marijuana card.
Related article: Is CBD Legal in the United States?
Medical marijuana does offer relief from chronic pain, and acts like other anti-inflammatory medications. The down side is, you have to register with the state and pay high fees. Insurance plans also don’t cover it – yet.
All the products that are manufactured by New Phase Blend fit the federal legal criteria and are considered THC free. They have less than 0.3% THC content, and come from the cannabis sativa (industrial hemp) plant.
Remember, the cannabis plant contains two sub-species: cannabis sativa (hemp), and marijuana. Marijuana products are still controlled, hemp products are not.
Choosing the Best CBD Anti-Inflammatory Products
When choosing what products to use, you should consider those that are safe, transparent, and of good quality. All the products should meet the following criteria:
- Made with organic hemp
- Pass tests for molds, pesticides, and heavy metals as recommended by the COA (certificate of analysis)
- Shouldn’t contain more than 0.3 % THC
Discover: CBD Oil for Arthritis
Other things you should consider include:
- The product’s potency
- Manufacturing processes and company certifications
Top CBD Products to Fight Inflammation
The following are some of the best anti-inflammatory CBD items you can use to help alleviate pain, swelling, and other forms of discomfort:
1. Soothe Potent Topical Anti Inflammatory Balm
Type: High strength CBD balm
CBD: 500mg, 1000mg, or 2000mg
Features: Full spectrum, lavender scented
Features
- 500 mg to 2,000 mg of CBD rich full spectrum hemp extract for quick anti-inflammatory results
- GMP certified production facility
- 100% organic hemp
- Lavender scent
- Specialized CBD topical formula that penetrates the skin quickly for immediate results
Want to experience the benefits of CBD oil, but in a topical form? If you’ve been looking for an effective CBD balm with outstanding anti-inflammatory properties, then this is definitely the product you should be going for. It’s a product line of effective CBD balms with a lovely lavender scent.
It’s manufactured using a full spectrum CBD, and it’s also mixed with other beneficial ingredients such as MCT oil (medium chain triglyceride), beeswax, hemp seed oil, and jojoba oil. The scent is magnificent- as is the functionality.
It’s hard to find another CBD of better quality than this topical balm. When making your purchase, you’re able to choose between 500 mg – 2,000 mg topical strength of a full spectrum CBD.
Full spectrum CBD is very effective when it comes to relieving general stress and tension in your muscles.
Apart from other types of muscle pain, you can also use it after exercising so you benefit from the anti inflammatory properties as a recovery agent.
As we mentioned earlier, it’s recommended that you start with the lowest effective dose, and slowly work your way up. Soothe is an effective cream that fully penetrates your skin hence allowing the dermis to absorb all the nutrients it has.
Related article: How Does Topical CBD Ointment Work?
You don’t have to wait too long to feel the effect of the balm after application. It gets to work quickly at address chronic pain associated with acute inflammation.
The scent is so amazing that you can treat it as a moisturizer like the many people who are already using it. Once you purchase it and use it, you’ll thank us.
As a high strength balm, Soothe combines well with other New Phase Blends tincture products. However, instead of waiting for the tinctures to absorb under your tongue in order to get to work, Soothe works by penetrating your skin to give you fast-acting results.
It deals with the problem from different angles making it a top competitor in the CBD oil industry. The performance of this CBD cream is guaranteed, too. If you aren’t happy with the results after purchase, you can return it within 30 days from the date you bought it. All refunds are typically conducted within 48 hours of receipt of the return item.
How long the topical balm lasts varies from person to person. For some users, the cream can last up to 6 hours. After application, you can expect to feel the effects for a couple of hours.
If it’s your first time using it, monitor the amount of balm you used and how long it lasts. You can adjust the amount as required.
When you use it for muscular aches and pain it might work much faster than when it’s used for joints; because the surface area covered by the skin around your muscles is much larger compared to joints.
2. Pure High Strength Vegan CBD Soft gel Capsules
Type: Pure CBD Softgel Capsules
CBD: 40mg per capsule
Features: Broad spectrum, vegan certified softgels
Features
- 40 mg per CBD oil capsule and 2400 mg of CBD rich hemp extract per bottle
- Contains 60 servings, take 1 CBD soft gel per day
- Broad Spectrum CBD (less than 0.3% THC)
- Non intoxicating
- Non addictive
- Plant based capsules
This is a vegan friendly option for CBD. The product has a relaxing and sedative effect on your body, and leaves you in a better mental state of well being. These vegan CBD capsules contain 40 mg of premium CBD rich hemp extract per CBD capsule.
New Phase Blends vegan CBD oil capsules use the purest CBD pills available on the market. If you’re looking for high quality vegan CBD oil capsules, this should be your first choice.
This product is very safe to use, it’s carefully made in a GMP (good manufacturing practice) certified facility. Therefore, the products are consistently produced as well as controlled according to quality standards.
The hemp used in the manufacturing of Pure High Strength Vegan CBD Softgels is 100% organic, and it’s one of the highest quality hemp available across the world.
Every batch produced is usually tested by a third party organization that’s not affiliated to New Phase Blends in order to ensure quality.
It’s very important to trust the company you purchase CBD gel capsules from so that you aren’t sold under-dosed capsules or even fake ones. Yes, some companies do this to people. You need to be careful.
The capsules aren’t very different from using a CBD oil tincture. They contain a full spectrum hemp extract that’s rich in CBD. This product results in pain relief, anxiety relief, and more.
3. CBD Gummies for Sleep
CBD: 45mg per gummy
Features: Patent-pending CBD and melatonin formula for sleep
Features
- 45 mg of broad spectrum CBD extract per gummy
- 3 mg of melatonin per gummy
- 100% non psychoactive and non-addictive, each gummy contains less than 0.3% THC
- Provisional patent through the United States Patent & Trademark Office
- Tasty, wild cherry flavor
Chronic pain can be an inflammatory response that makes sleeping almost impossible. Being unable to sleep is a common problem among many people. These patent-pending CBD gummies for sleep help you deal with that.
They’re manufactured with premium, CBD rich hemp extract and melatonin. Remember, broad spectrum CBD products contain near 0.0% THC. Melatonin is naturally produced by your body. It’s a hormone that controls our sleep-wake cycles. New Phase Blends combines high quality melatonin with 100% organic hemp extract that has high amounts of CBN, CBG, and CBD to create the best gummies on the market.
Apart from helping you sleep, melatonin also has anti-inflammatory effects, it reduces inflammatory reactions in different ways. Didn’t know that melatonin could illicit this inflammatory response? Neither did I, to be honest. You can read more about it by clicking here.
By consuming these New Phase Blends gummies for sleep, you’re able to trigger your brain to inform your body that it needs to go to sleep much faster.
Our body’s receptors are indirectly regulated by CBD use. Therefore, it’s able to trigger a sequence of different responses all over your nerves, brain, and stem. These receptors can also help regulate neuropathic pain.
Related: The Differences Between Broad and Full Spectrum Explained
It doesn’t matter how severe your insomnia is, there’s a great chance these CBD gummies will help you sleep.
With the powerful combination of cannabinoids such as CBD and melatonin, going to sleep is much easier. They are part of New Phase Blends’ flagship product line, and widely viewed as the best gummies on the market.
You also get a money back guarantee if they don’t perform as advertised. The good thing about these sleep gummies is they are non-addictive, and won’t leave you feeling dazed in the morning.
On top of all the benefits, the wild cherry flavor adds a perfect touch to the gummies, making them easy to eat because of the amazing taste.
There are low chances of getting any side effects with these gummies. However, some of the rare side effects reported include headaches, nausea, and blood pressure.
If you prefer the same formula in CBD oil form, we have that as well. Check out the CBD oil for sleep.
4. Pure CBD Oil Drops
Type: Pure CBD Oil
CBD: 33mg or 66mg per serving
Features: Broad or full spectrum, premium CBD oil
Features
- 1,000-2,000 mg of CBD per bottle / 33-66 mg of CBD per serving
- You can choose between full spectrum CBD oil or broad spectrum CBD oil
- 30 servings @ 1 ml per serving size for a one month supply
- Includes 100% organic industrial hemp extract
- Non-psychoactive and contains less than 0.3% THC
This is one of New Phase Blends’ best-selling CBD oil products. It’s made with a CBD rich extract that results in a pure CBD oil – nothing less. This is, truly, a high quality CBD oil.
It helps with inflammation, anxiety, and other pains. You’re given the freedom to choose your flavor, strength, and spectrum. The MCT carrier oil includes very high percentages of essential fatty acids.
It makes for a premium organic CBD oil through the easy processing. The fats offer many benefits to the body, such as better high brain activity and energy in the form of fats that are readily available for the body to burn.
The product contains real CBD, therefore you won’t experience bad side effects. They’re also FDA approved hence are safe to consume. Only the best, pure CBD extract is used.
The third party lab results prove that it’s exactly what we claim it is. These premium CBD oil drops are made in a GMP certified facility.
You’ll enjoy outstanding results. Our CBD oil isn’t intoxicating, at all, because they contain only pure CBD from hemp. THC is what causes the psychoactive effects (found in marijuana, not hemp), and these contain less than 0.3% THC.
Summary – Anti Inflammatory Effects of Cannabidiol (CBD)
CBD oil products are a natural remedy that’s grown in popularity since it can be used to help with a number of ailments. Taking a CBD product offers a lot of benefits to your body, both mentally and physically. The effects of CBD have been studied over the years – this is nothing new. It’s only been recently legalized.
Related: What Do CBD Gummies Do For The Body?
Its’ potential role in easing symptoms of a number of health issues including acne, heart disease, anxiety, and depression is almost undeniable at this point.
CBD oil is a great remedy for inflammation and pain management, among other benefits. While THC is the component of marijuana that causes psychoactive effects, CBD doesn’t have such side effects.
A lot of users have reported positive results from using a CBD product for a variety of health conditions. CBD topicals, like a CBD balm, is effective when it comes to managing pain and skin conditions such as eczema.
If you’re seeking therapeutic benefits you should opt for full spectrum CBD oil that is potent and has organic ingredients in order to get the best results.
What are you waiting for? If you haven’t tried CBD products yet, well, it’s time to take a step in the right direction and use these wonderful products to deal with different issues you might be struggling with. There are many CBD oil companies out there, but our customers tend to conclude we are among the best in the industry.
References
Current Neuropharmacology: https://www.ncbi.nlm.nih.gov/
Journal of Cannabis Research: https://jcannabisresearch.biomedcentral.com/
National Conference of State Legislatures: https://www.ncsl.org/